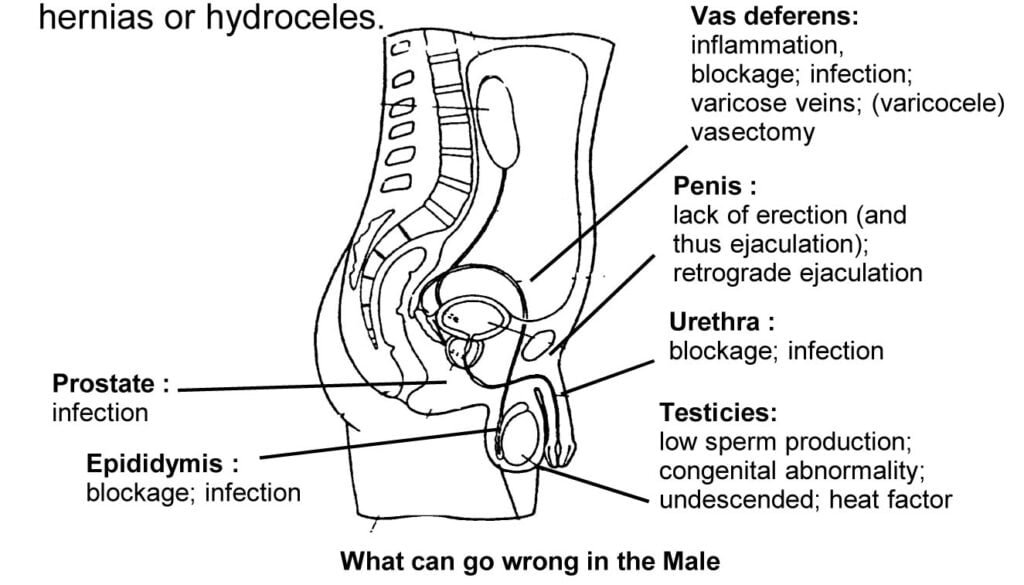
The commonest reason for male infertility is a low sperm count, and the commonest reason for this is what doctors call ‘idiopathic’—which simply means, we do not know! This is one of the reasons why the diagnosis of male infertility is so frustrating for both patients and doctors—there are very few tests available which allow us to pinpoint the cause of the problem. This drawback also means that there is very little in the form of effective therapy which we can offer these men’ if we do not know what is wrong, how can be treat it? However, what about those conditions which we understand? Let’s now discuss these conditions in details.
Varicocele
One of the commonest reasons for a low sperm count according to some doctors is a varicocele. A varicocele is a swollen varicose vein in the scrotum, usually on the left side. It usually causes no aches or pains. The condition occurs because blood gets pooled in the testicular veins (pampiniform plexus) since the valves in the veins are leaky and do not close properly. The reason for infertility associated with a varicocele are unclear. Perhaps the accumulation of blood causes the testes to become hot and thus damage sperm production; or the pooled blood brims over with abnormal hormones which may change the way in which the testes make sperm. The effect of the varicocele on an individual’s sperm count is variable; this may range from no effect whatsoever, to causing a very low sperm count. Varicocele may also have a progressively damaging effect on sperm production, so that the sperm count may decline with time.
How is a varicocele diagnosed? The doctor examines the patient in the erect position and feels the spermatic cord—the cord-like structure from which the testis hangs. The patient is also asked to cough at this time. A varicoclere feels like a ‘bunch of worms’ and, on coughing, this gets transiently engorged. Confirmation of this diagnosis is best done by a Doppler test at the same time. The instrument used in the Doppler test is a small pen-like ultrasound probe which is applied to the cord. This probe bounces sound waves of the blood vessels and measures the amount of blood flowing through the veins, and this can be recorded. Patients with a varicocele have a reflow of blood during coughing which shows up as a large spike on the tracing. Other somewhat uncommon tests which are done to confirm the diagnosis of a varicocele include: special X-ray studies, called venograms, and thermograms.
What are the areas of controversy regarding the varicocel? Most doctors are still not sure whether a varicocele causes a low sperm count or not! It is possible that the varicocele may be an unrelated finding in infertile men—a ‘red herring’. Strangely enough, only a quarter of the men with varicocles have an infertility problem. Thus, many men with large varicoceles have excellent sperm counts which is why correlating cause (varicocele) and effect (low sperm count) is difficult.
The foregoing contention means that surgical correction of the varicocele may be of no use in improving the sperm count ; after all, if the varicocele is not the cause of the problem, then how will treating it help? Nevertheless, surgery for varicocele repair is simple and straight forward; and since there is so little we can do in any case for most men with a low sperm count, most doctors will repair any varicoceles they find in infertile men. However, it should be kept in mind that varicocele surgery will result in an improvement in sperm count and motility in only about 50% of the patients. And it is still not possible for the doctor to predict which particular patient will be benefitted. Of course, merely improving the sperm count is not enough; and pregnancy rates after varicocele repair alone are around 25% only.
There are three methods available to repair varicoceles : conventional surgery; microsurgery; and radiologic balloon occlusion.
In conventional surgery, the most commonly performed procedure is as follows : a small cut is made in the groin; the spermatic cord is lifted out of the scrotum; and the engorged veins are tied off. In this case, the risks include: the risk of the varicocele recurring, which is about 20%, because some of the smaller veins are not identified and are missed out during surgery; the risk of formation of a hydrocele, i.e., a collection of fluid around the testes, because lymph vessels are indirectly tied off too, so that more fluid is accumulated (the risk is about 5%); and inadvertent damage to the testicular artery (the blood supply to the testis)—which can actually decrease sperm production!
Microsurgery is a newer method, in which under an operating microscope, the surgeon ties off individually the enlarged veins in the spermatic cord. The testicular artery and lymphatic ducts can be preserved confidently, because the surgery is done under high magnification.
Radiologic balloon occlusion is not very commonly performed. In this rather minor procedure, a silicone balloon catheter is passed under X-ray guidance upto the testicular vein. Here, the balloon is inflated and left in place permanently, thus blocking the engorged veins and repairing the varicocele.
Subclinical varicoceles are tiny varicoceles which cannot be felt by the doctor, but can be detected by Doppler examination. Whether correcting them is helpful or not is still a matter of individual opinion.
Many surgeons will combine varicocele repair with medical therapy to try to increase the sperm count by driving the testis to work harder, but the efficacy of this method is still not clear.
Duct Blockage
If the passage (reproductive tract) between the penis and testes is blocked, there will be no sperm in the semen (azoospermia). Blockages can be caused by infection (due to gonorrhea, chlamydia, filariasis, or TB) or by surgery done earlier to repair hernias or hydroceles.
A long and complicated two to three hour microsurgery called a vasoepididymal anastomosis (VEA) can be attempted to bypass the duct blockage. This surgery requires highly specialised skills and is best performed by an experienced microsurgeon, since the tubes involved are very fine and delicate. This surgery is technically difficult and intricate because it needs to be done under high magnification. The surgeon tries to bypass the block, so that the sperm can reach the penis.
Surgical results can be poor for the following reasons :
- Technical difficulty, because of the minute size of the tubes; often, potency cannot be restored, and the sperm count remains zero. The anatomic potency rate is about 50% for most patients (which means that sperm can be found in the semen after surgery).
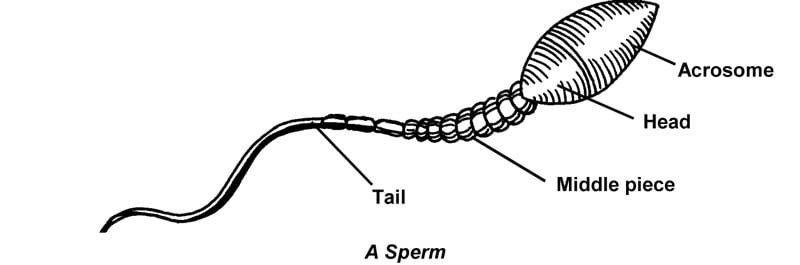
- The sperm are often poor in quality and are successful in giving rise to a pregnancy in only about 25% of the patients. This is because the sperm that make their way out may not be mature of motile since they have not spent enough time in the epididymis, which functions to mature the sperm in the body.
- Secondary damage to the epididymis and duct system may have occurred because they have been subjected to high pressure for a long time, causing multiple leaks and blocks, making surgery less successful.
- Damage to the functional lining of the epididymis may be present, either as a result of the infection which caused the block or as a result of the high pressure, so that it no longer works effectively and sperm cannot mature here properly.
The first surgical attempt offers the best chance of success; repeat surgery has a dismal success rate and is rarely worthwhile.
Congenital Absence of the Vas (the sperm-carrying tube)
For portients without a vas deference (a condition they are born with, but which can be diagnosed only much later on), the conventional treatment consisted of creating a pouch surgically, into which the epididymis was made to open. This pouch was called a spermatocele and sperm were aspirated from it and used for artificial insemination. However, pregnancy rates were very low. Recently, a technique developed by Dr Sherman Silber of USA allows some of the men (without a vas difference) to father a child. This technique is called MESA (microepididymal sperm aspiration), in which sperm are aspirated by microsurgery from the head of the epididymis and used for fertilizing the wife’s eggs in vitro by IVF.
Vasectomy
Men often undergo vasectomy to render then sterile once they have completed their family. Vasectomy is a simple, safe and easy surgical procedure which involves cutting the vas deference and sewing is shut, so that the sperm passage is blocked. These sperm are absorbed into the body so that although ejaculation is normal, there are no sperm present in the semen.
If the man changes his mind after a vasectomy, and wants to father another child, microsurgery can rejoin the cut ends so that the sperm can once more pass through into the semen. This reversal surgery is called vasostomy or VVA (vasovasal anastmosi). Such surgery is expensive and only a few doctors are adequately trained to perform the operation—and even then success is not guaranteed. The best results are obtained in those cases where the reversal surgery has been performed within 5 years after the vasectomy, i.e., before antibodies to the sperm are developed. Competent surgeons have reported pregnancy rates of as high as 80% in these cases.
Immunity Problems with Sperm
If varicoceles are controversial sperm, immunity problems are even more so! However, while the controversy surrounding varicoceles has not become quite old, the discovery of immune sperm problems is a relatively newer development, which means we have even more questions about these problems and even fewer answers!
In one of Nature’s quirks, men can develop antibodies to their own sperm or the wife can develop these against the husband’s sperm. What actually happens is that the man’s body’s defence mechanism destroys its own sperm; or the wife’s hostile cervical mucus does so, as though the sperm were enemy bacteria or virus. This can happen as a result of problems due to inflammation, injury to the testes, surgery, infection or blockage.
Problems start right from making the diagnosis. Antisperm antibodies are suspected to be present when the sperm are clumped to one another (agglutinate) while doing a semen analysis. A poor postocoital test, which shows that most sperm in the cervical mucus are immortile, is also a tip off, because one of the reasons for this finding is cervical mucus hostility due to the presence of antibodies.
Many test are available to detect antisperm antibodies. A blood test for antisperm antibodies can be done for both the wife and the husband using ELISA methods. This is an easy test to perform but interpreting the result is difficult—what does a positive test mean? Could it be responsible for infertility? Most doctors don’t think so, because they argue that the presence of these antibodies in the blood is of little clinical importance. But the debate still goes on! Antibody tests can also be done on the sperm itself, using immuno tests, which can tell the doctor whether the antibodies are present on the sperm head or tail.
Treatment for sperm immunity problems is equally confusing and includes administering testosterone injection to suppress sperm production; the rationale being that if there are no sperm there will be no further formation of the antagonistic antibodies.
Corticosteroids have also been used successfully to suppress the production of antibodies. But the side effects of these powerful drugs are several and quite adverse.
Other methods such as sperm washing to clean away the seminal fluid (which contains the antibodies) along with timed insemination, and IVF (in vitro fertilization) and GIFT (gamete intrafallopian transfer) can also be useful.
Hormone Imbalance
Unlike the the woman, hormone imbalance in the man is not a common cause of infertility problems. Hormonal problems can stem from organs as far apart as the brain or the testicles, and can show up in blood tests. Hormone imbalance can arise because of :
- Head injury.
- A tumour in the pituitary gland, at the base of the brain.
- A tumour in the adrenal gland, above the kidneys.
- Malfunctioning of the pituitary gland.
- Cirrhosis of the liver.
- Conditions present from birth, such as Klinfelter’s syndrome (47, XXY syndrome).
- A thyroid problem.
One uncommon problem is that of hyperprolactinemia (i.e., a high prolactin level). This problem is usually caused by a pituitary malfunction or tumour, and can be detected by a blood test. Patients with hyperprolactinemia often also have decreased libido and some may be impotent. Treatment with bromocryptine in order to suppress the high prolactin levels has proved highly successful in achieving pregnancy.
Another problem pertains to that of hypogonadotropic hypogonadism (poor functioning of the testes because of inadequate stimulation by the gonadotropic hormones (FSH and LH, produced by the ptiuitary gland). Most hypogonadotropic patients are hypogonadal; that is, their blood levels of testosterone, the male hormone, are low. This means that they have poorly developed secondary sexual character; an effeminate appearance; scanty hair; decreased libido; and small gabby testes. Such a condition can be confirmed by blood tests which show low levels of FSH and LH. This disorder can be treated by replacement therapy with the gonadotropin hormones, i.e., HCG (human chronic gonadotropin) and HMG (human menopausal gonadotropin). These are expensive injections and a fairly long course of treatment is needed before they begin to work, but they are effective in enhancing sperm production in these patients.
Substance Abuse
Not only are alcoholics unable to perform, but their liver function also deteriorates, resulting in excessive levels of the female hormone, estrogen, which has a severe sperm-suppressing effect. Drugs of abuse can also create malformed sperm with poor motility; they also alter hormonal balance and testicular function and cause impotence and erection problems.
Tobacco is a potent toxin. It attacks the tails of the sperm so that they are unable to swim effectively. The testicular artery can also go into spasms if it gets choked with nicotine and this decreased blood supply to the testis can also impair sperm production. Prolactin levels in smokers also tend to be higher, so sexual desire ‘disappears in smoke’.
Undescended Testes
Undescened testes are a tragic cause of male infertility, since often such a condition is preventable. Some babies are born with one or both testicles up in their bellies instead of hanging down in the scrotum. Sometimes the condition might correct itself by the time the toddler is around two years old. (Don’t worry unduly if you find the testes “occasionally disappearing” from the scrotum of a young boy. These testes are called “retractile” testes and are very common). However, if left unattended, the undescended testes tend to get damaged by the heat in the abdominal cavity and can even become cancerous in adult life. The child should be operated before two years of age or else fertility could be lost forever. Treatment with hormonal injections (HCG injections) to cause testicular descent is not alternative.
Torsion
If one of the testicles has undergone torsion (the doctor’s term for twisting), it could be damaged since it is deprived of its blood supply.
Signs of torsion are excruciating pain and swelling of the testicles. Sadly, it is often misdiagnosed as a testis infection, and left untreated. This inaction causes the testis on that side to shrivel up and die because it gets starved of blood (a condition called atrophy). The best way to confirm the diagnosis of torsion of the testis is to go in for a Doppler first. If confirmed, emergency surgery is needed right away, to untwist and fix the testis properly. The other testis also must always be fixed surgically to prevent it from undergoing torsion. Unfortunately, sperm antibodies are often produced which decrease sperm production in the other testis.
Infections
Earlier, the commonest reason for azoospermia in India used be smallpox. The smallpox virus attacked and damaged epididymis, causing ductal obstruction. Tuberculosis damages the epididymis, causing azoospermia. However, making a specific diagnosis of tuberculous epididymitis can be very difficult, because it is often a silent and indolent disease. Gonorrhea, chlamydia, syphilis and other STDs can also pay havoc with the male genital tract, causing irreparable damages to its epithelium (internal lining).
Strange as it may seem, mumps can also cause orchitis (inflammation of the testes), especially when it affects young men. Orchitis can cause severe damage to the testes, resulting in testicular failure.
What about other genital tract infections?
Many doctors will do a semen culture, to look for a treatable cause of infertility, of the semen sample shows many pus cells. If the test is positive treatment with antibiotics is instituted. Male reproductive tract infections (such as prostates) are often chronic and may require many weeks of antibiotic treatment. It is therefore important to recheck the semen culture after therapy, to ensure that the treatment has been adequate. However, the relation between the presence of bacteria in the semen and male infertility is still unclear. Do bacteria really cause infertility? Does treating the infection help to improve fertility? More questions than answers, once again!
Medication and Its effects
Some medications can play havoc with the sperm count or with the sex drive and these include : drugs for high blood pressure like resorting, methyldopa, guanethidine and propranolol; nitrofurantoin for urinary infection; corticosteroids; anabolic steroids for muscle building; and antipsychotic drugs.
A rare problem pertains to anticancer drugs and radiation therapy, which are used to treat young men suffering from cancers such as Hocking’s disease, lymphoma, leukemia and testicular tumours. In these men, the chemotherapy and radiation therapy used to treat the disease also wipe out sperm production, rendering them sterile. An option available today is to store the sperm (in sperm banks) which can later be used for inseminating the wife to achieve a pregnancy.
Detrimental Effects of Heat
The testicles have been placed in the scrotum because they can’t make sperm at body temperature—they need a cooler environment to do so. Consequently, they hang outside the body where the temperature is 0.80 C cooler. Tightly encased groins because of jock straps, tight jeans, lungottis and nylon briefs cause the testicles to be pressed back into the warmth of the body and literally ‘cook the sperm to death’ – especially when combined with hot tub baths and saunas. Heavy physical or manual labour, performed under hot conditions for long periods, like that in foundries, boiler plants and engine rooms, may also cause a lower sperm count as the testicles get too hot.
The damage due to the aforementioned factors can be prevented by wearing loose fitting cotton trousers and cotton boxer shorts, and by applying a cold towel soaked in ice water around the scrotum at least two or three times a day.
Occupational Hazards
Certain occupational hazards affect fertility by upsetting the hormonal balance, thereby suppressing sperm production.
Dangerous chemicals which have an adverse impact on fertility include the following : heavy metals, like lead, nickel and mercury; insecticides; petrochemicals; pesticides; benzene; xylene; anaesthetic gases, and X-rays.
Ejaculation Problems
Very often, a perfectly fertile man may not be able to ejaculate. Since he can’t make love properly he can’t make babies. Some men can’t even have an erection (impotence) and some cannot achieve an erection sufficient for intravaginal penetration or ejaculation in the vagina.
An older theory held that 80% of impotency problems (which are very common) were rooted in psychological inhabitation and fears which could respond to sex therapy and counselling. However, modern research has lowered this figure and estimates that 50% are due to physical causes ranging from inadequate blood flow to the penis, diabetes, neuralgic defects and hormonal problems.
How does the doctor suspect a physical problem? By asking a simple question : Does the individual have ‘wet dreams’? If men have nocturnal ejaculations (wet dreams), this would suggest that the physical apparatus is sound and that the problem is psychological.
Testing, in this context, includes nocturnal penile tumescence (NPT) testing, which monitors for normal night-time erections, and measuring blood flow through the arteries of the penis (using Doppler methods).
The treatment that may be prescribed includes :
1. Injections of papaverine and prostaglandins (chemicals which cause blood vessels to dilate) can be self-injected into the penis under medical supervision. These substances increase the blood flow to the penis, thus creating an erection.
2. A surgical implant or penile prosthesis to give an artificial erection.
3. Microsurgery to plug leaks in the veins of the penis, thus preventing the loss of turgidity of the erect penis.
The sperm of an individual can also be collected by masturbation and used for artificial insemination. This procedure has a very high success rate, because there is really no fertility problem as such for the patient.
Retrograde Ejaculation
Retrograde ejaculation means that the semen goes backwards into the bladder instead of coming out of the penis, so that very little or no semen is ejaculated at the time of orgasm; and the urine looks cloudy after having sex. This phenomenon occurs when the bladder sphincter muscle does not contract properly during orgasm, as a result of which the semen leaks back from the urethra into the bladder. This condition could be caused by prostate surgery, a spinal injury, diabetes, high blood pressure medication and congenital problems.
A simple way to diagnose retrograde ejaculation is to examine a man’s urine after he ejaculates. If there are sperm present in the urine, this confirms the diagnosis.
Self-help in such a situation includes trying to have sex with a full bladder and while standing up, because this mistakes the muscle around the opening of the bladder more likely to stay closed. Some medications like decongestants can also help the sphincter muscle to close. Surgery can also be performed on the opening of the bladder to event it from misbehaving, but such a method is not very successful.
An effective treatment option is to collect the sperm and use it later for artificial insemination. After emptying the bladder, the man alkalinizes his urine by drinking soda bicarbonate and then urinates immediately after ejaculation. The sperm in the urine are recovered by special laboratory processing techniques and used for insemination. Pregnancy rates with insemination are usually low because the recovered sperm are often of poor quality and sometimes these sperm have to be used for IVF to GIFT so as to give a reasonable chance for pregnancy to occur.
Electro-ejaculation for Spinal Cord Problems
Men with spinal cord problems who cannot ejaculate can now father a child with the help of a new technique called electro-ejaculation. In this technique, a probe is inserted into the man’s rectum and electrical stimulation is delivered to the prostate in a gradually increasing fashion to induce and ejaculate. The man usually attains an erection and ejaculates in about five minutes. The sperm recovered from this ejaculate can then be used for intrauterine insemination (IUI), IVF or GIFT, depending upon their quality (which is usually poor).
Treating the Couple
As we have seen in this chapter, if the man has a low sperm count, little can be done with conventional therapy to improve this condition. A better way is perhaps to improve the women’s fertility potential using the method of superovulation (helping her to grow many eggs). It might seem unfair that the woman is being treated for what is, essentially, the man’s problem, but the fact of the matter is that there is very little effective therapy for a low sperm count and the medicines available at present are much more effective allopathic for treating the woman, though ayurveda and homoeopathy are effective in low sperm count. Since the fertility of the couple is the sum of the fertility potential of both the partners, a male factors problems can often be treated by treating the female!
Conclusion
Conventional treatment of male infertility has poor success rates and leaves a lot to be desired. However, the availability of assisted reproductive technology in recent times has revolutionized our approach to male infertility, and using techniques such as IUI, IVF, GIFT and microinjection, many men can be helped to father their own babies. This is a rapidly developing area and spectacular advances have occurred in recent times.

