I.B.S. is a functional disorder. It responds poorly to a biomedical philosophy of management and must be understood in the context of the patients psychological and social environment.
Irritable bowel disease is likely to be sub-divided into various groupings with different aetiologies.
Abnormal Gut Motility
Diarrhoea, constipation or a pattern altering between these two is characteristic of IBS, and led to the theory that intestinal dysmotility is the primary disorder. Pain and abdominal bloating which often accompany these symptoms, could then be due to enteric smooth muscle spasm and impaired intestinal clearance of gas.
This theory sounds plausible, but no distinctive pathophysiology of intestinal motor function has been identified. However, intestinal motility is complex and difficult to examine directly. It is possible that abnormal neuromuscular signalling, which cannot be detected by current technology, may be found in some patients with IBS.
Gut Hypersensitivity
There is more evidence supporting the theory that patients, with IBS have altered responsiveness to a range of afferent stimuli— they have supersensitive intestine. This effect is demonstrated by a crude but useful test for IBS—which rectal distension with air during sigmoidoscopy can reproduce the patient’s pain. This has been studied further using controlled hydrostatic distension of the colon by intraluminal balloons. Patients with IBS had a lower pain threshold than the control group.
A number of other stimuli have been found to produce gut symptoms at lower thresholds in patients with IBS, including:
Some mental and physical stressors.
Gut peptides.
Cholinergic stimuli.
Bile acids.
Dietary fats.
The evidence for afferent hypersensitivity is generally more compelling than for a primary motor disorder.
Psychosomatic cause
Most of them have some form of phychopathology. The most common diagnosis are anxiety and/or depression, yet the evidence that these are primary problems and that the gut sympotms are secondry is not very compelling—depression is slightly more likely than anxiety to be a primary problem.
A number of studies have measured psychological stress, and their results have supported many patients’ self-reported experience that sympotms are worse at time of stress. However, more rigorous studies have found that the association is weaker than clinical experience suggests. Study results are inconsistent, and a recent multivariate analysis has actually found lower levels of stress in IBS patients than in controls! However, stressful life events probably increase the likelihood of hospital referral.
Food Intolerance
Some patients with lactose intolerance secondry to mucosal hypolactasia have IBS-like symptoms, and may benefit from milk withdrawal. However, lactose deficiency is not increased in IBS.
Possible aetiological factors in irritable bowel disease are as follows :
- Primary disorder of gastrointenstinal motility
- Hypersensitivity of gut mucosa
- Psychological problem
- Food intolerance
- Specific trigger
- Gastrointestinal infection
- Drugs
- Pelvic surgery
It has been suggested that there is a much larger group of patients with a wider range of food intolerance. Although there is no reliable laboratory or immunological test for food intolerance, doubleblind food challenges have identified patients with IBS whose symptoms improve if the offending foodstuff are excluded. However, this finding can only be regarded as indirect evidence for the role of food intolerance in the pathogenesis of IBS.
Specific Triggers
Some patients can link the onset of symptoms to external factors, such as gastroenteritis or antobiotics. Hysterectomy occasionally precipitates IBS in women.
There are certain life events too which may trigger IBS:
- Death of a parent
- Leaving home
- Marriage
- Having children
- Break down of a relationship
- Unemployment
- An abusive experience
Clini cal picture of IBS
The characterstic features of IBS are well known. The manning criteria were the first attempt to diagnose IBS from the patient’s history. They were derived from a study of a group of patients with IBS who were given a list of 15 symptoms and asked which ones they had. Six symptoms were closely correlated with the diagnosis of IBS. The more symptoms a patient has, the more likely he is to have IBS.
Rome criteria for the diagnosis of IBS : At least three months’ continuous or recurrent symptoms of Abdominal pain or discomfort which is :
- Relieved with defaecation
- And/or associated with a change in frequency of stool
- And/or associated with a change in consistency of stool
- And two or more of the following on at least a quarter of occasions or days:
- Altered stool frequency
- Altered stool
- Altered stool passage
- Bloating or feeling of abdominal distension
Other symptoms associated with IBS:
- Indigestion
- Heart burn
- Tiredness
- Backache
- Headache
- Dizziness
- Breathlessness
- Frequent Urination
Minimum investigation for IBS :
- Full blood count
- Erythrocyte sedimentation rate
- Multi-channel biochemistry
- Sigmoidoscopy
- Rectal biopsy (especially if patient has diarrhoea)
The reliability of Manning’s criteria has been confirmed in subsequent studies. They have formed the basis for the Rome symptom criteria which are now used as diagnostic criteria for clinical studies.
Making the diagnosis
Patients presenting with bowel symptoms should have a thorough history and examination, as well as selective investigation. When taking the histrory, general practitioners should be aware of any factors that could increase the likelihood of the patient having a functional problem.
A prolonged series of tests can cause unnecessary anxiety. It is useful to tell the patient that the result of investigation are likely to be normal, so that the subsequent explanation that tests are normal becomes a positive experience.
INVESTIGATION GUIDELINES
It is difficult to formulate guidelines on when to proceed to barium enema or colonoscopy. With increasing experience and confidence, the need for the physician (as opposed to the patient) to be reassured declines.
The length of history and the age of the patient are the most common factors influencing the decision to image the colon. We tend to do a colonoscopy in patients with predominant diarrhoea, as this group has a greater chance of organic pathology than those other patterns of altered bowel habit.
Dietary Advice
The traditional advice to eat a high-fibre diet may be good theoretically, but has proved to be virtually useless in various. This lack of benefit has been confirmed by clinical studies.
Patients often ask for dietary advice and may offer a list of aggravating foodstuffs. There is no reason why they cannot try subtracting specific foods. Particularly committed patients may work through an exclusive. One can take the help of a dietician.
Summary
- Ten to fifteen percent of the population have symptoms of the irritable bowel syndrome, and the prevalence is higher in women.
- Although IBS has traditionally been a diagnosis of exclusion, modern management emphasizes the need to make a positive diagnosis.
- Patients with IBS who are referred to OPOs are more likely to be anxious and have neurotic symptoms than those treated in the community.
- It is probable that, as its genesis is better understood, IBS will be sub-divided into various groupings with differing aetiologies.
- Characterstic clinical features of IBS include abdominal pain, disturbance of bowel habit, bloating and passage of mucus through rectum.
- It is helpful to tell the patient that the result of investigations are likely to be normal, so that the subsequent explanation that tests are normal becomes a positive experience.
- Management should include a sympathetic explanation, a trial of diet, and constitutional symptomatic treatment
Psychological Approaches
In addition to a conventional approach, counsellor, phychologist or psychiastrist may be consulted. Some patients seem to respond to hypnotheraphy.
Psychological Treatments Useful in IBS :
- Hypnotherapy
- Cognitive Behavioural therapy
- Psychodynamic psychotherapy
- Anti depressents
Excersises and Yoga
A specific exercise for flatulence, acidity, heartburn and heaviness in the stomach is as follows:
After every meal lie down first on your right side. Take deep breath eight times. Turn and lie down on your back and take 16 deep breaths, now turn to your left side and deep breathe 32 times.
Asanas like Vajrasana, Padmasana, Parvatasana, Pavanamuktasana, Bhujangasana, Dhanurasana, Matyasana and Yogamudra are specific for Digestive Disorders. All these are described in a separate chapter.
Hydrotherapy
Take a thin cloth, say a hand-towel, of the required size according to the area of application. Dip it in ice cold water and squeeze out the water to prevent dripping. Frequent changing of the compress is necessary before it gets warm. In order to make the compress last longer, a thicker compress will serve better. It must be pressed firmly in place.
Very cold applications are given with ice chips filled in a rubber bag with screw cap. If ice-bag is not available, woollen or flannel can be used instead. The pack must not drip. The area to be treated must be covered with a towel and the pack should be placed above it. This is useful for abdominal pain.
Hip Bath
Hip bath is given mainly for abdominal disorders. It can be given sitting in an ordinary bath tub with the legs on the sides of the tub or in a tub which can accommodate a person to sit comfortably with the legs resting on the floor.
Procedure
Fill the tub with hot water enough to cover the hip. The temperature of the water should be as per the individual’s tolerance. A brisk massage should be given frequently to the abdomen as long as one in the bath. The duration of the bath can be from 5-15 minutes. After coming out of the bath splash or spray cold water and dry-briskly with a coarse towel. Hot hip bath is useful in constipation, piles, obesity, distended stomach, poor digestion and worms.
A cold hip bath can be given similarly for better circulation of the internal organs of the abdomen, and for the same duration. At the end of the bath do not splash or spray water but give a vigorous rub with a thick towel and scrub dry.
Cold hip bath is useful for the same disorders as hot hip bath when used alternating the former.
Internal bath
Enema is the water treatment given to the bowels and rectum. Giving enema in all diseases is an essential part of Naturopathy.
The uncleared morbid substance inside the bowels is effectively removed by enema. When the bowels are clean, the severtity of the disease automatically reduces. By taking enema the muscle tone of the bowels and rectum increases and its healthy movement is restored.
For perfect cleansing, enema is preferably given in the morning after the evacuation. However, in cases of constipation, enema is given first thing in the morning.
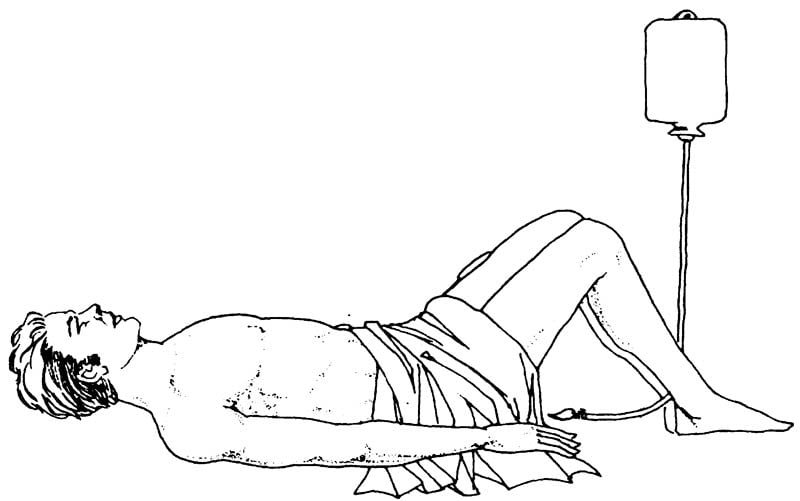
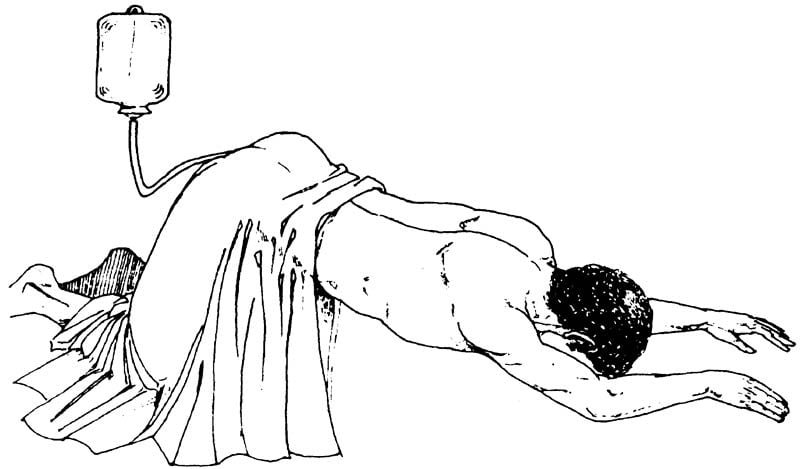
Enema is given in three conventional positions, lying down on the left side, lying on the back with knees raised and stooping forward in a standing position with knees bent. A thorough cleasing cannot be obtained in the squatting position or sitting on toilet bowl.
Method of giving enema
Assume the desired position. Suspend the enema pot filled with half a litre of pure tap water, one metre above. Apply a little oil or vaseline to the nozzle of the rectal tube. Before insertion check the rectal tube to ensure free flow of water. Insert the tube into the rectum. The flow of water can be adjusted with the knob attached to the tube. When all the water has been jected, remove the tube and resist the pressure for a few minutes. The bowels can be emptied after a while for better cleansing. If one does not wish to take enema in the lying position, he can take it in the standing position.
Enema can be given with benefit during fever, for constipation and almost in all diseases.
Home Remedies for different symptoms of IBS are:
Stomach-Ache (abdominal pain)
- For immediate relief, powder one tsp. of ajwain (carum) and half tsp. of jeera (cumin) and mix in warm water. To this add the juice of half a lemon and a pinch of rock salt and drink it at least twice a day.
- Mix 4 gms. pudina (spearmint), half tsp. each of saunf (fennal seeds) and along with a pinch of rock salt and heeng (asofoetida). Take it with warm water twice daily.
- Cut a lemon into half and add to it some rock salt, kala jira (Black caraway) and pepper and suck it slowly.
- Boil four tender neem (Margosa) leaves in water, strain it and add two black peppercorns, a pinch of rock salt and drink twice a day.
- Dry and powder the outer skin of a pomegranate and eat half tsp of the powder with honey twice a day.
- Mix half a tsp. of the juice of tulsi (basil) leaves with one-fourth tsp. of juice of ginger and drink with warm water.
- Mix one tsp. of juice of jamun (Jambul) with rock salt and drink it.
- Take a pinch of powdered chotti harar with warm water.
- Powder some mustard seeds and apply on the stomach for instant relief of pain and vomiting.
- Drink half tsp. of crushed garlic with warm water.
Foods to be avoided
- Fibrous fruits and vegetables.
- Spicy foods.
- Fatty foods.
- Meat, fish, etc.
- Pulses, beans and other pulses which cause the formation of gas in the stomach.
Indigestion
- Take one tsp of lemon juice, half tsp of crushed ginger, a small amount of coriander leaves, mint, one black pepper, a pinch of cumin and salt and grind it into a paste. Take this paste either half an hour before meals or immediately after meals.
- Take 200 gms. of carum, 4 gms. of hing and 20 gms. of rock salt and powder them. Take 2 gms. of this powder twice a daily with warm water after meals.
- To one glass of fresh water, add juice of a medium sized lemon and drink it after every meal.
- Take half tsp each of juice of lemon and onion after each meal.
- Add roasted cumin, black pepper and salt to buttermilk and drink after meal.
- Add equal amounts of juice of ginger, lemon and orange and drink after each meal.
- Drink tomato juice to which rock salt is added, twice daily.
- To one tsp. each of carrot juice and juice of spinach, add two pinches of rock salt. Take this preparation early in the morning daily.
- Make a chutney of mint leaves and add asafoetida, curtain, black pepper, carum and salt. Eat this after every meal.
- Take a ripe papaya, cut it into small pieces, eat after adding salt, pepper and lemon juice to it.
Hyperacidity/Heart burn
- Drink coconut water daily to fight acidity.
- Take a few coriander leaves, crush and mix them in water. To this, add a pinch of rock salt and drink twice daily.
- Add two pinches of powdered chotti harar to honey and swallow twice daily.
- Mix one tsp juice of amla, one fourth tsp of roasted and powdered cumin, half tsp of powdered cariander seeds and a small piece of mishri (sugar candy) and take it once daily after meals.
- Take a small amount of spinach, five pieces of parwal and boil together. Add a few drops of juice of coriander leaves and salt. Cool this juice and drink twice daily. This improves the burning sensation and eructation.
- For acid eructation, take two tsp of juice of radish and add some mishri and take it twice daily.
- Chew one clove after meals, this will reduce the acidity.
- Drink one glass shrerbat of gulkand twice daily.
- Take a few seeds of bathua saag and powder them. Take 2 gms of this powder with honey once daily. This keeps the bowel clean and removes excess acid.
- Take a few leaves of pipul tree. Dry and powdered them. Take one tsp of this powder with water once daily.
Foods To be avoided
- Stale food.
- Spicy and oily food.
- Sweetmeats.

