Some pregnant women are considered to be at ‘higher risk’ than most women. They include women who have diabetes, heart disease or high blood pressure or who develop these condition during pregnancy or labour. They also include women who are carrying their fifth or later child; who are carrying more than one baby; who are under 17 or over 35; who are over 30 and carrying their first child or who develop signs of preterm labour. The degree of risk varies with each of these conditions and should be thoroughly explained to you by your doctor.
If you are in a higher-risk category, the management of your pregnancy and labour may need to be varied from that of a low-risk woman. Consequently, not all of the options discussed in this book may be available to you.
Some of the more common conditions that place women in the higher-risk category are discussed below.
Gestational Diabetes
Diabetes is a condition characterized by a high level of sugar or glucose in the blood. Diabetes that occurs only in pregnancy is known as gestational diabetes. During pregnancy, hormones cause the woman’s insulin to be less effective at metabolizing glucose. The resulting high blood sugar can lead to complications in both the woman and baby. The condition disappears after pregnancy for the vast majority of women, although a third of afflicted women become gestational diabetics with subsequent pregnancies. In later life, they are also more likely to develop non-insulin-dependent diabetes. Most women who are well controlled during pregnancy have good pregncies and healthy babies.
Warning Signs
The following symptoms may be warning signs of complications during pregnancy:
- Vaginal bleeding. It is never normal to bleed during pregnancy.
- Sharp abdominal pain or severe cramping.
- Loss of fluid from the vagina.
- Any signs of labour before the thirty-seventh week of pregnancy.
- Persistent nausea or vomiting.
- Frequent dizzy spells or fainting.
- Visual disturbances such as dimness, blurring, flashes of light or dots in front of the eyes.
- Sudden and excessive swelling of the face, hands or feet.
- Severe and persistent headache.
- Pain or burning upon urination.
- Marked decrease in the frequency of urination.
- Persistent dull or sharp pains, anywhere.
- Fever higher than 100F orally or chills and fever.
- Vaginal discharge that is irritating.
- Noticeable decrease in foetal movement.
- Any other problem that you feel is unusual.
If you experience any of the above symptoms, contact your caregiver as soon as possible.
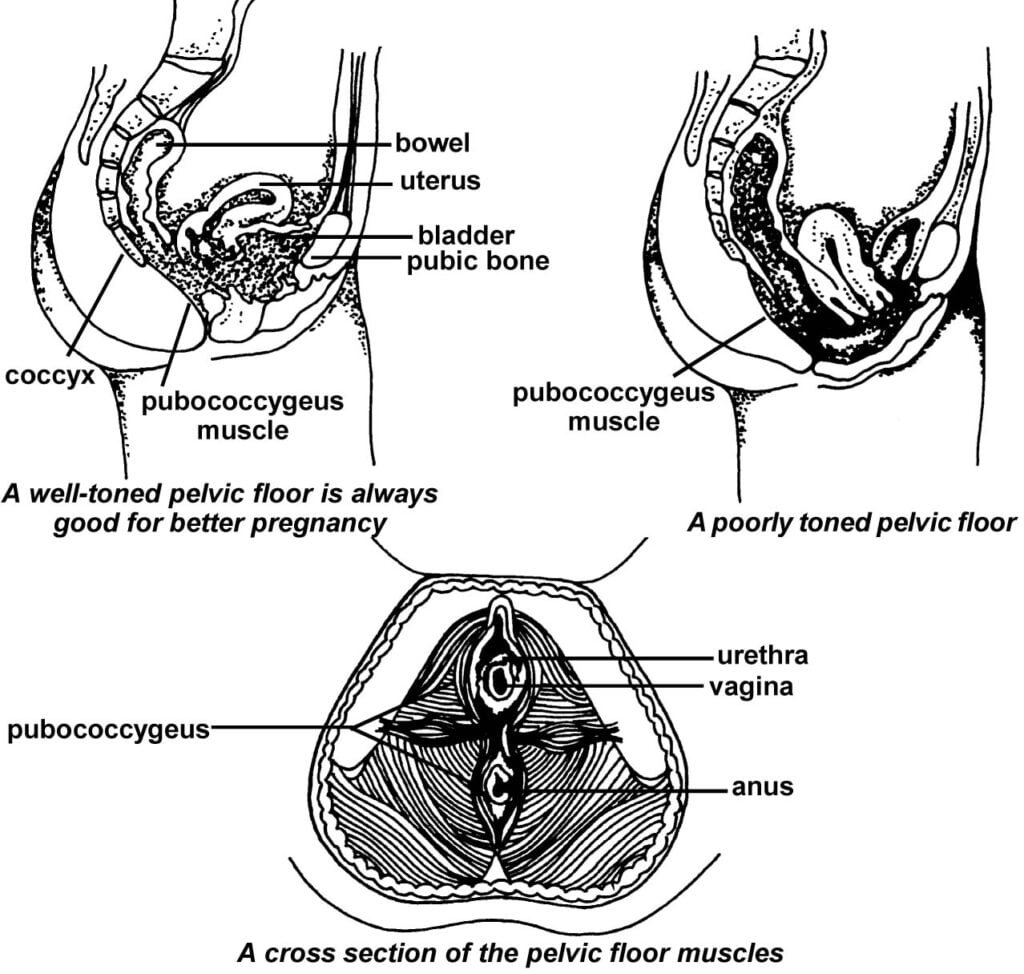
Note : Before getting pregnant, consult your gynaecologist for exercises to tone up pelvic floor. The risk factors for developing gestational diabetes are family history, previous large babies or previous gestational diabetes. The condition is more common in women who are obese or over the age of 25. Most practices screen all women at 28 weeks for the condition with the glucose tolerance test. Once a positive diagnosis is confirmed, the pregnant woman is placed on a diabetic diet. Home monitoring of blood sugar is performed several times a day. If diet alone does not control the blood sugar, insulin may have to be given. The babies of untreated diabetic women may be very large, making delivery more difficult. Other complications include respiratory difficulties, jaundice, a low level of calcium in the blood and stillbirth. If the diabetes is not controlled, hypoglycemia (low blood sugar) may occur after birth. While in uterus, a baby produces high levels of insulin to absorb the woman’s high blood sugar. At birth, the woman’s supply of sugar drops and the baby’s high level of insulin may cause his own blood sugar level to drop very low. Nursing soon after birth helps to prevent hypoglycemia. Women who have diabetes are more likely to develop pregnancy-induced hypertension. To prevent stillbirths, their doctors may induce labuor before or on the due date. If the induction is not successful, a cesarean section is performed. Infection and postpartum haemorrhage are also more common in diabetic women.
Pregnancy-Induced Hypertension
Hypertension (high blood pressure) that occurs during pregnancy is called pregnancy-induced hypertension (PIH). Most women who develop PIH did not have hypertension before pregnancy and will not have it after. PIE was formerly known as toxaemia. While the cause of PIH is unknown, some studies suggest that the blame lies with an imbalance of the substances that regulate the constriction and dilation of the blood vessels. The risk factors include heredity, a diet low in protein or calcium, a history of preeclampsia prior to 32 weeks gestation, chronic high blood pressure, kidney disease, lupus, diabetes, multiple pregnancy, age (under 20 or over 35) and being overweight. A new theory states that PIE may be—an immune response to a new sex partner, since 85 percent of cases occur in first-time pregnancies. Several studies have shown that a good diet can reduce the risk of developing PIH. A diet containing 75 to 100 grams of protein and 1,500 to 2,000 milligrams of calcium is recommended.
PIH affects both the woman and the fetus. High blood pressure constricts the blood flow to the uterus. This can result in the baby receiving less oxygen and nutrients, which will affect his growth. In addition, the placenta may separate from the wall of the uterus before delivery and result in bleeding and shock. If untreated, PIH can become preeclampsia, which is characterized by high blood pressure, protein in the urine, sudden weight gain and swelling of the face and hands. It may be necessary to induce labour if the blood pressure is not controlled. This may lead to a premature infant. Rarely, preeclampsia progresses to eclampsia, which is marked by convulsions, coma or even death of the woman or baby.
Treatment of PIH consists of bed rest for mild conditions. Occasionally, a woman must be hospitalized. If the blood pressure is not controlled, delivery by induction of labour or cesarean section may be necessary to save the lives of the woman and baby. The medication magnesium sulfate is administered intravenously to prevent convulsions. The risk of seizures diminishes 48 hours after delivery of the baby.
Multiple Pregnancy
If you are pregnant with more than one baby—with twins, triplets, or more your pregnancy is called a multiple pregnancy. Fraternal twins are more common than identical twins and are the result of two sperm fertilizing two eggs. Fraternal twins may or may not be the same sex and are no more alike in appearance than any other siblings. Identical twins occur less frequently and are the result of one sperm fertilizing one egg, which then separates. Since identical twins carry the same genetic material, they are always the same sex, always look alike, and always have the same blood type. They may be mirror images of each other.
During pregnancy, an increased demand is placed on the body of a woman carrying more than one baby as well as additional placentas or one larger placenta. The discomforts of pregnancy are accentuated, since there is an increased demand on the circulatory system and the uterus is larger in size. The chances of PTH and preterm labour are greater. For these reasons, many physicians place these women on bed rest at around 28 weeks gestation.
Women experiencing a multiple pregnancy have higher protein and caloric requirements. Additional protein is necessary to provide for adequate growth of the babies and to ensure good muscle tone of the overdistended uterus. Women who eat well during pregnancy decrease their chances for complications and increase their chances for delivering at term.
Preterm Labour
If a baby is born before the thirty-seventh week of pregnancy—more than 3 weeks early—the birth is called preterm and the baby premature. Preterm birth represents the greatest health risk to newborns. Preterm babies have an increased risk of neonatal problems. Their lungs and other organs may not ready to function yet. Respiratory distress is the greatest concern and the babies often have difficulty maintaining their body temperature. In addition, their sucking may be weak, and they are more susceptible to infection.
Women who are more likely to go into preterm labour include those who had a previous miscarriage or preterm birth; who have an overdistended uterus from a multiple pregnancy or from an excess of amniotic fluid; who smoke, take drugs or are malnourished; who are under the age of 18 or over 35; who are experiencing a high degree of emotional distress; who have jobs that involve standing for long periods or enduring other stressful working conditions and who have a vaginal or urinary tract infection or an infection of the membranes of the amniotic sac.
Preterm labour can often be stopped if it is caught in time. The treatment for preterm labour includes bed rest; antibiotics, if indicated, for infection and possibly medications to relax the uterus and stop the contractions. While some studies question the efficacy of bed rest, it is the current treatment of choice.
The U.S. Food and Drug Administration (FDA) recently approved a test that can predict whether a pregnant woman is about to experience a preterm birth. The test detects a substance called foetal fibronectin in the cervical/vaginal secretions. Foetal fibronectin is an adhesive protein that serves as a ‘natural glue’ on the placenta. The substance changes into a lubricant just before labour begins. It should not be present in the cervical/vaginal secretions after the twenty-second week of pregnancy unless there is a problem, such as preterm labour or an infection. Its presence indicates a high risk of delivering within the next 2 weeks.
In cases of impending preterm birth between 24 and 34 weeks gestation, a treatment is available that accelerates foetal lung maturity. Synthetic steroids have been shown to reduce the incidence of respiratory distress syndrome and brain hemorrhage in newborns by 50 percent and to reduce death rates by 40 percent. According to a recommendation of the National Institute of Health (NIH), this medication should be used when delivery prior to 34 weeks gestation is likely, unless the medication will have an adverse effect on the man or delivery is imminent.
If you experience any signs of labour more than 3 weeks before your due time, contact your caregiver right away.

